Health tech Austin is a gathering of Leaders and Innovators from Texas and beyond.
We are an essential part of the health care ecosystem in Texas, with connections across the country. We host health care conferences, networking events and competitions.
Our constituents are thought leaders, start-up executives and other stakeholders interested in taking on the big issues in health care and working on solutions.
We nurture creative thinkers and doers.
IF YOU ARE INTERESTED IN SPONSORING A FUTURE EVENT;
CONTACT:
HELLO@HEALTHTECHAUSTIN.COM
SPONSORED BY HUSCH BLACKWELL
A DIFFERENT KIND OF LAW FIRM. ONE WHERE TRAILBLAZING LEADERSHIP AND INVENTIVE APPROACHES DELIVER UNMATCHED PERSONAL SERVICE AND EXPERT GUIDANCE, HELPING YOU PURSUE YOUR MOST AMBITIOUS GOALS.
THE INNOVATION ROUNDTABLE
THOUGHT LEADERS AND INNOVATORS ARE COMING TOgether TO SHARE THEIR KNOWLEDGE, EXPERIENCE, AND INSIGHTS ABOUT THE INTERSECTION OF AI, LAW & HEALTHCARE
FEATURED SPEAKERS
Charles “Charley” Taylor, PhD, is one of the world’s foremost experts in the application of computational science to the practice of medicine. His research on the use of artificial intelligence and computational methods transformed the practice of cardiology and gave rise to the field of predictive, simulation-based medicine.
Taylor is the co-founder of HeartFlow, where he developed a noninvasive tool that uses imaging to simulate and assess blood flow through the coronary arteries — the first AI-enabled technology to be included in cardiology clinical practice guidelines. In 2023, NEJM AI recognized it as the most widely adopted AI technology in U.S. health care.
In 2024, his pioneering work in computational biomechanics earned him election to the National Academy of Engineering.
Taylor started his career at Stanford University, where he received his Ph.D. in mechanical engineering. He served as a founding faculty member of the Department of Bioengineering, with additional appointments in surgery, mechanical engineering and radiology.
Taylor holds bachelor’s and master’s degrees in mechanical engineering as well as a master’s degree in mathematics from Rensselaer Polytechnic Institute.
To date, Taylor’s research has resulted in 450 peer-reviewed journal and conference papers and has been funded by the National Science Foundation, National Institutes of Health, U.S. Food and Drug Administration, Defense Advanced Research Projects Agency and the American Heart Association. He holds 300-plus U.S. and international patents.
Ganesh Padmanabhan is the CEO and founder of Autonomize AI, a technology company transforming healthcare knowledge workflows with AI Agents and Copilots. Autonomize AI’s products organize, contextualize, and summarize unstructured healthcare data, enabling knowledge workers to make data-driven decisions that improve patient outcomes and drive impactful change in the industry.
A seasoned business leader, entrepreneur, and investor, Ganesh brings deep expertise in data and artificial intelligence (AI). He is a passionate advocate for using technology to tackle humanity’s biggest challenges and believes in the power of AI to augment human potential. Ganesh is dedicated to the ethical use of AI and data, championing technology as a global equalizer to create opportunities for all.
Ganesh also founded Stories in AI, a podcast and an edu-tainment platform that explores the transformative impact of AI through storytelling. His prior roles include scaling venture-backed AI companies like Molecula and CognitiveScale and leading growth initiatives during a 15-year career at Dell Technologies and Intel Corporation.
In addition to leading Autonomize AI, Ganesh is an investor and advisor for multiple startups and an active mentor in the Austin, Texas entrepreneurial ecosystem. He served on Texas Governor Greg Abbott’s COVID-19 Strike Force on Innovation in 2020, where he helped leverage data for decision-making during the state’s pandemic response.
A frequent keynote speaker, Ganesh has been featured in Forbes, Business Insider, Fast Company, and other leading publications. He was recognized by Enterprise Management 360 as one of the 10 tech experts revolutionizing AI as AI was maturing in 2018. Ganesh holds a bachelor’s degree in Mechanical Engineering from the University of Calicut, India, and an MBA from the McCombs School of Business at the University of Texas at Austin.
Adam Royal, JD counsels healthcare industry clients on issues covering virtually the entire spectrum of corporate, transactional and regulatory law. Adam’s transactional practice covers M&A and joint ventures with specific experience on the regulatory aspects of business formations and combinations in the healthcare industry.
He routinely advises clients on regulatory compliance and provides strategic advice to executives, compliance teams, and risk professionals on a range of legal, business, and governance topics including healthcare contracting and negotiation, the Anti-Kickback Statute, Stark Law, HIPAA, Medicare billing, and government audits and appeals.
Genentech's Legacy and Future Aspirations are Built on the Belief that the boundaries of science are meant to be broken and that we can solve some of the hardest biomedical challenges plaguing humankind.
Penalize UnHealthy EATING/Encourage Healthy vs
My Plate. My Choice
Genetic Testing vs Protecting Privacy
LSD: New Hope For Mental Illness vs.
Psychedelics Are Too Dangerous
bonus session: audience participation
THOUGHT LEADERS AND INNOVATORS came TOGETHER TO SHARE THEIR KNOWLEDGE, EXPERIENCE, RESEARCH, AND INSIGHTS ABOUT brain & Mental Health
———————————————————————————————————————————————————————
THE AGENDA
8:00 am Breakfast & Networking
Opening Remarks
Alyssa Aguirre
Board Chair
Alzheimer’s Association
Capital of Texas
Beyond the Silos: Collaborating for Collective Impact to Drive Better Mental Health Outcomes
Moderator
Nicole Clark, PhD
Anchor
Spectrum News
Calvin Kelly, PhD
Chief Clinical Officer
Harvest Trauma Recovery Center
Clarena Tobon
Executive Director
NAMI Central Texas
Innovations In Public Mental Health
Jeff Richardson
Chief Executive Officer
Integral Care
Understanding the State of Texas Budget: Navigating Healthcare's Impact
The Honorable Glenn Hegar
Comptroller
State of Texas
Catalyzing Transformation in Brain & Mental Health: Innovating in Tech, Care Delivery, and Business Simultaneously
Moderator
Jason Scharff
Founder
Austin Next
Marianne Fazen, PhD
President/CEO
Texas Business Group on Health
John Forrest
Co-Founder/CEO
Veravas
12:00 pm Networking & Departure
summit SPEAKERS
Alyssa Aguirre is the Assistant Director of Dementia Care Transformation at The University of Texas Dell Medical School and Assistant Professor of Practice at The University of Texas Steve Hicks School of Social Work. She has dedicated her career to designing new models of Alzheimer’s disease and related disorders (ADRD) care, advancing palliative care research, and providing direct patient care to individuals living with ADRD and their family care partners.
Alyssa received the Sojourn Scholar Leadership Award from the Cambia Health Foundation for her leadership, and in 2023, she was appointed as a Faculty Scholar with the NIA IMPACT Collaboratory Faculty Scholars program to support ADRD initiatives within the health care systems.
Alyssa’s current research is focused on validating innovative care partner assessment tools and using machine-learning techniques to support ADRD family care partners. She received her Master’s in Social Work from the University of Michigan in 2009, having received a Specialist in Aging Certificate. She proudly serves as the Chair of the Board of Directors at the Alzheimer’s Association Capital of Texas Chapter and holds an Interdisciplinary Teams and Healthcare Certificate from Boston University.
Dr. Nicole Clark is an Emmy award-winning anchor and reporter for Spectrum News in Texas. She feels honored to work for an organization that values credibility and is dedicated to creating diverse coverage and giving everyone a voice on the issues that matter most to them. Nicole is inspired by her deep love for people and their unique experiences. More so, Nicole considers anchoring the afternoon and evening news as a dream job, allowing her to explore a diverse list of topics, share the news of the day, talk to change-makers, and give viewers a deeper understanding of issues that affect them.
Prior to Nicole’s impressive journalism career, she spent almost two decades in the Psychology field. The recipient of several educational degrees, including a Ph.D. in Counselor Education, an MS in Behavioral Science, and a BA in Psychology. Nicole also worked as a PhD-level psychotherapist for over 15 years.
Before joining the Spectrum News team, Nicole spent time working at various stations across the country, winning several awards along the way. A well-respected and decorated journalist, Nicole has won four Associated Press awards, including Best Daytime Newscast, a Louisiana Association of Broadcasters award for Best Political Coverage, and two Emmy awards for Interview/Discussion and Education/Schools. In addition, she was also chosen as Best News Anchor in Monroe, Louisiana, and Austin, Texas.
Dr. Calvin A. Kelly, Chief Clinical Officer at the Harvest Trauma Recovery Center is a Licensed Mental Health Professional and Certified Psychological Forensic Evaluator in Austin, Texas.
He has over 28- years of teaching experience in the fields of Psychology and Counseling courses both at the undergraduate and graduate level, and twenty-seven (27) years of experience in
private practice as a psychologist and Certified Trauma Expert. In addition to his distinguished teaching career, Dr. Kelly has had an extensive history in university administration. He has served an Associate Vice Chancellor in the University of North Carolina System; and most recently as a Dean at St. Edwards University .
As a clinician, student affairs professional, and educator, Dr. Kelly has had the opportunity to practice and refine his leadership skills and style. His style of leadership is based on the Servant Leadership Model. He has also been afforded the opportunity to present on a variety of topics nationally that are
related to his area of expertise and interests in mental health.
Dr. Kelly’s areas of interest and expertise include but are not limited too; trauma and post-traumatic stress related issues; Racial Identity Development; diversity and inclusion issues; men and depression;
secondary trauma; holistic wellness; organizational development and leadership; and team building.
Dr. Kelly feels strongly that it is his belief in family and close spiritual connection that keeps him grounded and focused.
Clarena Tobon is the Executive Director of NAMI Central Texas and a dedicated advocate for mental health. With over eight years of experience in nonprofit leadership, including key roles at United Way and Habitat for Humanity, Clarena has a proven ability to drive meaningful change. Her advocacy work has taken her to Congress twice, where she spoke with the American Foundation for Suicide Prevention.
Clarena’s personal connection to mental health is deeply rooted in her own lived experience, having lost her mother to suicide and now serving as a caregiver to her two school-aged children who face mental health challenges. This loss fuels her passion and underscores the importance of the work she does every day. She is committed to breaking the stigma and expanding support for those impacted by mental health conditions.
Outside of her professional life, Clarena cherishes time spent with her children, whether exploring new culinary experiences or planning their next adventure together.
Jeff Richardson is the Chief Executive Officer of Integral Care in Austin TX and the former Vice President and Chief Operating Officer of Sheppard Pratt, a prominent behavioral health organization in Maryland. Serving over 70,000 people across 380 locations, Jeff demonstrates exceptional leadership in the behavioral health sector. His impressive career includes a twenty-three-year tenure as the Executive Director of Mosaic Community Services, highlighting his dedication to community-based care.
Jeff holds a master’s degree in social work from the University of Maryland and a master’s in business administration from Loyola University. His commitment to behavioral health advocacy is evident through his involvement in nonprofit boards and state task forces. Jeff has held prestigious roles such as Board President for The National Council for Behavioral Healthcare and President of the Board for the Mental Health Association of Maryland.
Furthermore, Jeff’s contributions to the field extend to consulting, publications, and presentations on critical behavioral health topics, including systems redesign, business development, community mental health, strategic planning, affordable housing, healthcare technology, clinical services and nonprofit mergers and acquisitions.
Beyond his professional achievements, Jeff is a devoted family person, married with four adult children, one of whom has special needs. This personal experience fuels his passion for providing effective and quality behavioral health services to individuals and families facing similar challenges.
The Honorable Glenn Hegar was elected Texas Comptroller of Public Accounts in 2014 and was re-elected in 2018 and 2022.
Hegar is a sixth-generation Texan who grew up farming land that has been in his family since the mid-1800s. He’s a 1993 graduate of Texas A&M University and earned his law degree at St. Mary’s University. Before his election as Texas Comptroller, he served in the Texas House of Representatives and Texas Senate, where he worked on issues including public education, transportation, tax reform, government transparency, Second Amendment rights, water issues and tort reform.
As comptroller, Hegar is chief finance officer for the world’s eighth-largest economy. He has emerged as a passionate advocate for conservative financial management who focuses on his agency's constitutional duties and is committed to maintaining its reputation for customer service and transparency. He founded the state’s Transparency Stars program, pushed for ways to protect our Rainy Day Fund against rising inflation, worked to reform our state pension systems and guided the formation of the nation’s first state-administered precious metals depository. Hegar is recently working toward closing Texas’ digital divide and remediating the opioid crisis, through the Broadband Development Office and Opioid Abatement Fund Council, respectively.
His upbringing taught him the core values of hard work, honesty and integrity — the same values he and his wife Dara work to instill in their three teenagers, Claire, Julia and Jonah. Hegar’s most important title throughout his years of service is the one closest to home: Dad!
Jason Scharf is an experienced strategy executive and active angel investor in the life science and digital health sectors. He has built and led teams in strategic planning, market intelligence, and innovation.
In an era where biology, tech, and business intersect, Jason offers a unique blend of strategic foresight, entrepreneurial acumen, and incisive questioning. Through key roles at industry leaders like Illumina, Keen Health, Becton Dickinson, and Amgen, Jason has honed a systems-thinking approach, turning complex data into actionable insights.
As an angel investor, Jason has backed game-changing startups in Digital Health & Tech Bio sectors. The portfolio includes Pleno, Iridia, Abterra Biosciences, Syntrillo, and Elicio Therapeutics—a recent Nasdaq exit. These investments reflect Jason's commitment to the convergence of technology and biology, consumer-driven health solutions, and the rise of the Texas Triangle as the next bio innovation hubs.
Beyond his investment activities, Jason hosts the Austin Next Podcast. The show explores Austin's emergence as an innovation powerhouse, delves into broader technology shifts, and uncovers the underlying mechanics of innovation ecosystems. Jason's writings on Austin's Bio+Health scene, venture capital, and global trends are catalyzing important conversations.
Marianne Fazen, PhD is President and CEO of the Texas Business Group on Health, a statewide organization representing Texas employers in healthcare purchasing and policy issues, and Executive Director of the Dallas-Fort Worth Business Group on Health, a regional coalition of DFW area employers and healthcare organizations committed to improving healthcare quality, affordability, and accountability in North Texas.
Ms. Fazen is a frequent speaker and commentator on employer-sponsored health benefits and healthcare issues. She has been recognized as a member of the Dallas 500 Business Leaders by D CEO Magazine for the past 5 years and as a DFW Healthcare Leader by the Dallas Business Journal’s Who’s Who in Healthcare.
Ms. Fazen currently serves in leadership positions in several national healthcare organizations, including Regional Director of The Path Forward for Mental Health & Substance Use, Regional Leader of the national Leapfrog Group for Patient Safety, and Board Member of Equest Equine Therapy. Previous leadership positions included: Past President of URAC, a national healthcare accreditation organization, Board of Governors and Past President of National Alliance of Healthcare Purchasing Coalitions, representing 40 regional employer coalitions across the country, including TBGH and DFWBGH, and Executive Committee of the North Texas Accountable Healthcare Partnership, a multi-stakeholder collaborative to transform healthcare delivery in North Texas.
Ms. Fazen has a Bachelor’s Degree in Medical Technology from University of Wisconsin and a Doctorate in Communications Science & Human Development from University of Texas at Dallas.
John Forrest is a seasoned entrepreneur and visionary leader with a 30-year track record in driving global healthcare IT and innovation. His relentless focus has always been on leveraging technology to elevate patient care and profoundly impact lives.
Throughout his career, he has established companies that enhance access to high-quality healthcare information and testing, recognizing the critical role of timely and accurate diagnostic test results. He has achieved Inc. 500 fastest growing company list and won a Stevie Award for app design to automate patient workflow and achieve optimal outcomes.
In his current capacity as Co-Founder and CEO at Veravas, he has channeled his passion towards effecting positive change for individuals faced with Alzheimer's Disease and various neurodegenerative conditions. Veravas is at the forefront of early disease detection with a break-through blood test to detect Alzheimer’s up to 10 years prior to symptoms.
Thought Leaders and Innovators
came Together To Share Their
Knowledge, Experience, Research, and Insights
About The Future Of health.
THE AGENDA
7:45 am Networking & Breakfast
Opening Remarks
Hugh Forrest
Co-President/Chief Programming Officer
SXSW
Special Remarks
Claire England
Investment Partner
GPG Ventures
FEATURED SPEAKERS
Benjamin Isgur
Vice President
Health Care Thought Leader
Fidelity Health
Craig Watkins, PhD
Executive Director
IC2 Institute
UT-Austin
Chris Finberg
Innovation Director
PATHS-UP
Texas A&M University
Kirsten Ostherr, PhD
Professor/Founder
Medical Future Labs
Rice University
Charles Silver, JD
Professor/
Endowed Chair
UT-Austin
12:00 pm Networking & Departure
FEATURED SPEAKERS
Hugh Forrest serves as Co-President and Chief Programming Officer for South by Southwest (SXSW). For his role of Chief Programming Officer, he oversees content for the SXSW Conference, as well as the SXSW Music Festival, the SXSW Film Festival and SXSW EDU.
Forrest was named "Austinite of the Year" in 2012 by the Austin Chamber of Commerce (along with fellow SXSW Directors Roland Swenson, Louis Black and Nick Barbaro). In 2014, Forrest and these other SXSW Directors were named Austin Entrepreneurs of the Year by Ernst & Young. He received an honorary doctorate of humane letters in 2018 from Kenyon College, his alma matter. In 2021, he was awarded Diversity Champion of the Year by the Austin Black Business Journal.
In addition to his work at SXSW, he has previously served on of the National Advisory Board for the Poynter Institute in St. Petersburg, Florida. He has also served on the Board of Directors for Austin Habitat for Humanity. He currently sits on the Board of Directors for the Austin-based accessibility company Knowbility. Via his decades of work with the Austin Reggae Festival, he has helped to raise more than $1 million in funding for the Central Texas Food Bank.
Before joining the SXSW team in the dark ages of 1989, he founded a small monthly alternative publication called The Austin Challenger. He also wrote for several other newspapers and publications, including the Austin Chronicle, the Texas Sports Chronicle, the West Austin News, Willamette Week and the Seattle Weekly.
For 2024, SXSW is scheduled March 8-16.
A seasoned investor with executive experience, Claire England is Investment Partner with GPG Ventures, a healthcare venture capital firm with more than 100 portfolio companies nationally. GPG opens venture-ready investing opportunities in the $4.3 trillion U.S. healthcare market to family offices and individuals, who invest in companies directly alongside the firm's partners.
The firm is built on more than 60 years of healthcare, operational, and financial experience with an extensive syndicate investor network and offices in Dallas, Houston, and Austin.
In addition to GPG, she's a partner in two Portfolia funds, Food & AgTech and FemTech I, where she made 22 investments, and a partner in an impact investing advisory firm, LOHAS.
She’s also a Kauffman Fellow (a global innovation program and network of 882 VCs and LPs) and a member of Private Equity Women Investor Network, or PEWIN. She serves on St. Edward’s University’s Business School Advisory Board, and she received the 2018 Kauffman Fellows Leadership Award.
S. Craig Watkins, PhD is the Ernest A. Sharpe Centennial Professor and the Executive Director of the IC2 Institute at the University of Texas at Austin. His research focuses on the equity implications of computer-mediated technologies. Craig is one of the Principal Investigators for UT-Austin’s Good Systems Grand Challenge, a University funded initiative that supports multi-disciplinary explorations of the technical, social, and ethical implications of artificial intelligence. Craig’s team explores the racial equity implications of artificial intelligence, focusing on how implicit biases, for example, in datasets, model formulation, and deployment can lead to disparate impacts, especially in high stakes contexts such as healthcare and policing.
His collaborative research with Design and the School of Information examines how Black and Latinx children interact with AI-consumer devices like digital assistants. Craig was also part of multidisciplinary team of social scientists, psychologists, and computer scientists who prototyped a chatbot to support parents dealing with postpartum depression. Craig leads a team that is adopting a data-oriented approach to understanding the social determinants of health. This current research has led to the design of an AI-based solutions to mitigate the mental healthcare crisis in the U.S
Craig is an internationally recognized expert in media and technology systems and the author of six books and numerous articles and book chapters. His work has been profiled in places as varied as the Washington Post, Atlantic, Newsweek,TIME, ESPN, NPR, and featured at venues like SXSW, The Aspen Institute, The Boston Federal Reserve, New York Hall of Science, MIT’s Media Lab, and The New York Times Dialogue on Race.
Kirsten Ostherr, PhD, MPH is the Gladys Louise Fox Professor of English and Director of the Medical Humanities Research Institute at Rice University in Houston, Texas. Kirsten is the author of Medical Visions: Producing the Patient through Film, Television and Imaging Technologies (Oxford, 2013) and Cinematic Prophylaxis: Globalization and Contagion in the Discourse of World Health (Duke, 2005), and editor of Applied Media Studies (Routledge, 2017). She is founder of the Medical Humanities program (2016-present) and the Medical Futures Lab (2012-present), and she has extensive experience using human centered design for patient collaboration in health technology development.
Her research on trust and privacy in digital health ecosystems has been featured in Marketplace Tech on NPR, The Atlantic, STAT, Slate, and The Washington Post. Her writing about the COVID-19 pandemic has been featured in The Washington Post, STAT, and Inside Higher Ed. She is currently writing two books: Virtual Health, and The Visual History of Computational Health. Kirsten leads a digital health humanities project called “Translational Humanities for Public Health,” and her work was recently profiled in The Lancet.
Kirsten’s research is supported by the the National Institutes of Health, the National Endowment for the Humanities, the National Library of Medicine, the National Humanities Center, and the Andrew W. Mellon Foundation.
Mr. Chris Finberg is the Innovation Director for the National Science Foundation sponsored Engineering Research Center called PATHS-UP (Precise Advanced Technologies and Health Systems for Underserved Populations) The Center is a collaborative effort with Texas A & M, UCLA, Rice, and Florida International Universities. The goal is to create new & innovative technologies and health systems for point-of-care use to address Diabetes and Cardiovascular Disease in the underserved populations.
The Center is taking a development approach quite unconventional to academia by engaging with stakeholders from all sectors - investors, healthcare providers, physicians, patients, communities, and industry- throughout the R&D process. Mr. Finberg is originally from the Minneapolis area where he received his Mechanical Engineering degree from the University of Minnesota. He spent his entire career in industry with the last decade working in the medical device industry with contract manufacturing companies. Specifically with Class III long term implantable devices for Cardiac Rhythm Management (CRM’s) and Neuromodulation. Working with companies like Medtronic, Boston Scientific, Abbott/St. Jude, Biotronik, LivaNova and others.
Today Mr. Finberg’s role is to create an Innovation Ecosystem to insure the technologies created and develop at the Center continue on to scalability and commercialization. That is being done by fostering entrepreneurship with students and faculty, working with start-up companies, building an Industry Consortium where large, medium, and small companies across the entire value chain, and build on those relationships to further innovation - with the ultimate goal of helping those underserved populations have a healthier life.
Charles Silver holds the Roy W. and Eugenia C. McDonald Endowed Chair in Civil Procedure at the School of Law, University of Texas at Austin, and an Adjunct Scholar at the Cato Institute.
His recent writings on health care law and policy include Overcharged: Why Americans Pay Too Much For Health Care (Cato Inst. 2018), coauthored with David A. Hyman, and Medical Malpractice Litigation: How It Works—Why Tort Reform Hasn’t Helped (Cato Inst. 2021), coauthored with Bernard S. Black, David A. Hyman, Myungho Paik, and William M. Sage.
He is currently working on a proposal to the use Medicaid expansion as an opportunity to conduct a pilot project in which, instead of paying providers to treat beneficiaries, the program would deposit funds into health savings accounts that beneficiaries would use to purchase medical treatments directly. The project is described in “Leveraging The Medicaid Expansion,” University of Pennsylvania Journal of Law and Public Affairs (forthcoming 2024) (with David A. Hyman).
He earned his JD Yale University, Master of Arts from the University of Chicago, and Bachelor of Arts from the University of Florida.
Ben Isgur has spent more than 25 years guiding US and global health benefit leaders and decision makers with industry intelligence and research-based perspectives. His work informs business leaders on the interdependencies between the health industry, benefit trends and the employee experience.
An author, Ben has written numerous reports, which have been cited by leaders across the health industry. He is frequently interviewed and quoted by journalists from media organizations such as The New York Times, The Wall Street Journal, The Washington Post, The Economist, and Modern Healthcare. He is an accomplished speaker, and has given keynote addresses on diverse topics, from the drivers of US medical cost trend to the rise of the healthcare consumer’s voice.
Prior to joining Fidelity Investments, Ben founded a health research institute for a global consulting firm, where he led a team of industry experts, policy analysts and economists dedicated to developing original and independent thought leadership. Ben also developed health policy as a legislative director in the Texas House of Representatives and as a government relations officer for the City of Austin.
Ben received a master's degree from the LBJ School of Public Affairs at the University of Texas at Austin where he was a US Department of Defense fellow. Ben is a fellow with the American College of Healthcare Executives and serves as a board member for multiple health-related not-for-profits.
PRESENTED BY HUSCH BLACKWELL
A DIFFERENT KIND OF LAW FIRM. ONE WHERE TRAILBLAZING LEADERSHIP AND INVENTIVE APPROACHES DELIVER UNMATCHED PERSONAL SERVICE AND EXPERT GUIDANCE, HELPING YOU PURSUE YOUR MOST AMBITIOUS GOALS.
—————————————————————————————
HEALTH CARE FIGHT CLUB WAS A FAST-PACED SERIES OF DEBATES FEATURING THOUGHT LEADERS GOING HEAD TO HEAD ON HOT-BUTTON ISSUES IN HEALTH CARE.
IT WAS A FUN, FESTIVE, EDUCATIONAL, ENLIGHTENING, NETWORKING-FILLED EVENT.
Jason Scharf
The Champion
Health Care Fight Club
Serena Bumpus
The People's Choice
Health Care Fight Club
The Honorable Donna Howard
Texas House District 48
The Judges
Harold Strong
Dr. Jacob Childers
Rebekkah Schear
Lamarque Polvado
End of Life Care vs. Medical Aid in Dying
Value-based Care vs. High-Quality Care
More Physicians vs.
More Nurse Practioners & Physician Assistants
AI innovation vs AI Regulation
The Referees
Jason Scharf has spent nearly two decades catalyzing innovation in the Bio and Health space, taking on key leadership roles in strategy and market intelligence at industry pillars Illumina, BD, and Amgen.
His teams transformed complex data into actionable insights and plans, significantly shaping the strategic direction of these companies. As an Angel Investor and Advisor, Jason has a keen focus on nurturing the growth of the bio innovation tech stack and digital health startups.
Hosting the Austin Next Podcast, Jason explores the evolution of Austin into a superstar hub plus the dynamics and nature of innovation. Jason’s quest to answer “What’s Next?' extends to his writings, where he explores similar themes across technology, business, and life sciences.
Serena Bumpus, DNP, RN, NEA-BC is the CEO of the Texas Nurses Association. Bumpus is a long-time member of TNA and has held several volunteer roles as well as serving as the Director of Nursing Practice & Professional Development from 2020-2021.
Her career spans more than 20 years, with the last 12 in nursing leadership positions. Most recently she served as Senior Regional Director of Clinical Surveillance for Ascension Health. She holds an associate degree in nursing from Austin Community College and bachelor’s, master’s and doctorate in nursing from Texas Tech University Health Sciences Center.
She holds advanced certification as a nurse executive from the American Nurses Association (ANA). As CEO, Bumpus leads the strategic direction of TNA and its Foundation as well as represents the state at the national level with ANA.
Dr. David Zuniga is a licensed psychologist in private practice in Austin, Texas, and specializes in serving hospice and palliative care patients, their families, and medical caregivers. Previously, he was a faculty member in the Integrative Medicine Department at The University of Texas MD Anderson Cancer Center.
In addition to his PhD in clinical psychology, he earned an M.Div. from Harvard Divinity School in comparative religion, is a Zen Buddhist Priest and Vice-Bishop in one of the oldest lineages of Korean Zen, and worked as a hospice/hospital chaplain for over a decade.
He also holds an MA in English literature, is a former newspaper columnist, and has a fellowship with Fielding Graduate University to write a book on the intersections of Zen, mindfulness, and psychology related to trauma, wellness, and end-of-life care.
Dr. Zuniga has been interviewed and profiled by numerous media outlets such as Public Radio International, NPR, PBS, ABC, NBC, CBS, Fox News, and the Clear Channel Radio Network, and he has published widely and spoken internationally at leading academic conferences on Zen, mindfulness, psychology, and healthcare-related concerns: www.drdavidzuniga.com.
Cesar Lopez is the Texas Hospital Association’s VP, Legal Affairs, manages all aspects of THA’s internal and external legal matters, and assists with state and federal advocacy efforts before the Texas Legislature and regulatory agencies.
Before joining THA, Cesar was a part of the legal team at Group Health Cooperative (now Kaiser Permanente of Washington), in Seattle, WA, and worked with the Washington State Hospital Association, MultiCare Health System, and The Polyclinic (a large physician-owned practice).
A Rio Grande Valley native, Cesar earned a BA from Trinity University, a JD from Albany Law School, and an LLM in health law from the University of Washington School of Law.
Janis Powers has 20 years of experience in healthcare as a strategy consultant (Deloitte, Avanza Healthcare Strategies), thought leader (author of the bestseller Health Care: Meet the American Dream) and entrepreneur (founder of the digital health platform KnowThyself).
Janis advocates for improving the quality of the American healthcare system by reducing bureaucracy, customizing patient care, empowering patient choice, standardizing pricing and decentralizing the payment system. She has a B.A. from Yale and an M.B.A. and M.Arch. from the University of Michigan.
Steven Cutbirth leads all marketing and communications efforts for Scene Health, a medication engagement company using meaningful person-to-person connections via async video to solve one of the most serious problems in healthcare: medication nonadherence.
Prior to his role at Scene, Steven was head of marketing at Point Health (Formerly The Karis Group), a digital health company making healthcare easy to find, easy to understand, and easier to afford. Steven also served as Director, Digital Analytics and Engagement at Real Chemistry (formerly W2O Group), directly partnering with clients to identify actionable insights from complex data sets and create insights-based marketing & communications strategies. Client work included Aetna, CVS Health, Bayer, Houston Methodist Hospital, Baylor Scott & White, Optum Health, & Merck.
Steven holds a BBA in Marketing & Management from Baylor University, an MBA in Economic Development from Eastern University, and an MS in Healthcare Transformation from the Value Institute for Health and Care at The University of Texas at Austin, a joint venture between Dell Medical School and the McCombs School of Business.
Dr. Cliff Porter is the managing partner and founder of Texas Direct Medical Care. He is board certified in Family Medicine with the experience to provide highest level of personal medical care for our guests.
Prior to opening Texas Direct Medical Care, Dr. Porter was medical director for several urgent care clinics in Travis County. Before settling permanently in Austin, Dr. Porter was an Army physician stationed at Ft. Hood, practicing full-service family medicine, taking care of all ages of active duty soldiers and their families, including retirees in primary care, hospital admissions, emergency medicine, intensive care, as well as obstetrics, delivering babies in the middle of the night.
Dr. Porter served with 1st Armored Division, deployed to Iraq in 2011, and served part-time in the Texas Army National Guard as the senior flight physician for aviation (36th Combat Aviation Brigade).
Dr. Porter has joined the growing physicians adopting the Direct Primary Care model, revolutionizing primary care. Our model allows us to provide the best personal care for all of our guests.
John Moore is a seasoned healthcare IT analyst and the Managing Partner of the boutique analyst firm, Chilmark Research. Beginning his career as a genetics researcher at world-renowned labs in Massachusetts, John found his way to healthcare IT when he decided to pursue his first startup in the behavioral health space, RxApps, which was accepted into both the Rock Health and Startup Health accelerators before eventually folding.
Seeing the vast potential for new information technologies to drastically improve the science of medicine and process of care delivery, John joined Chilmark Research full-time after RxApps to help guide the industry in effective development and implementation of these solutions to realize their full transformative potential.
At Chilmark, John develops the company's research agenda with input from other analysts and clients on which topics are most in need of timely information about the market trends and drivers impacting solution adoption and buying behavior. Current research focuses on the emerging solutions that address different use cases for real-world data and evidence, responsible development of AI, omnichannel approaches to both care delivery and patient engagement, and solutions enabling the ongoing transition to value-based care. In addition to developing the company's research, John also produces the Chilcast podcast and brought together the collaborative Health Impact Project in 2023.
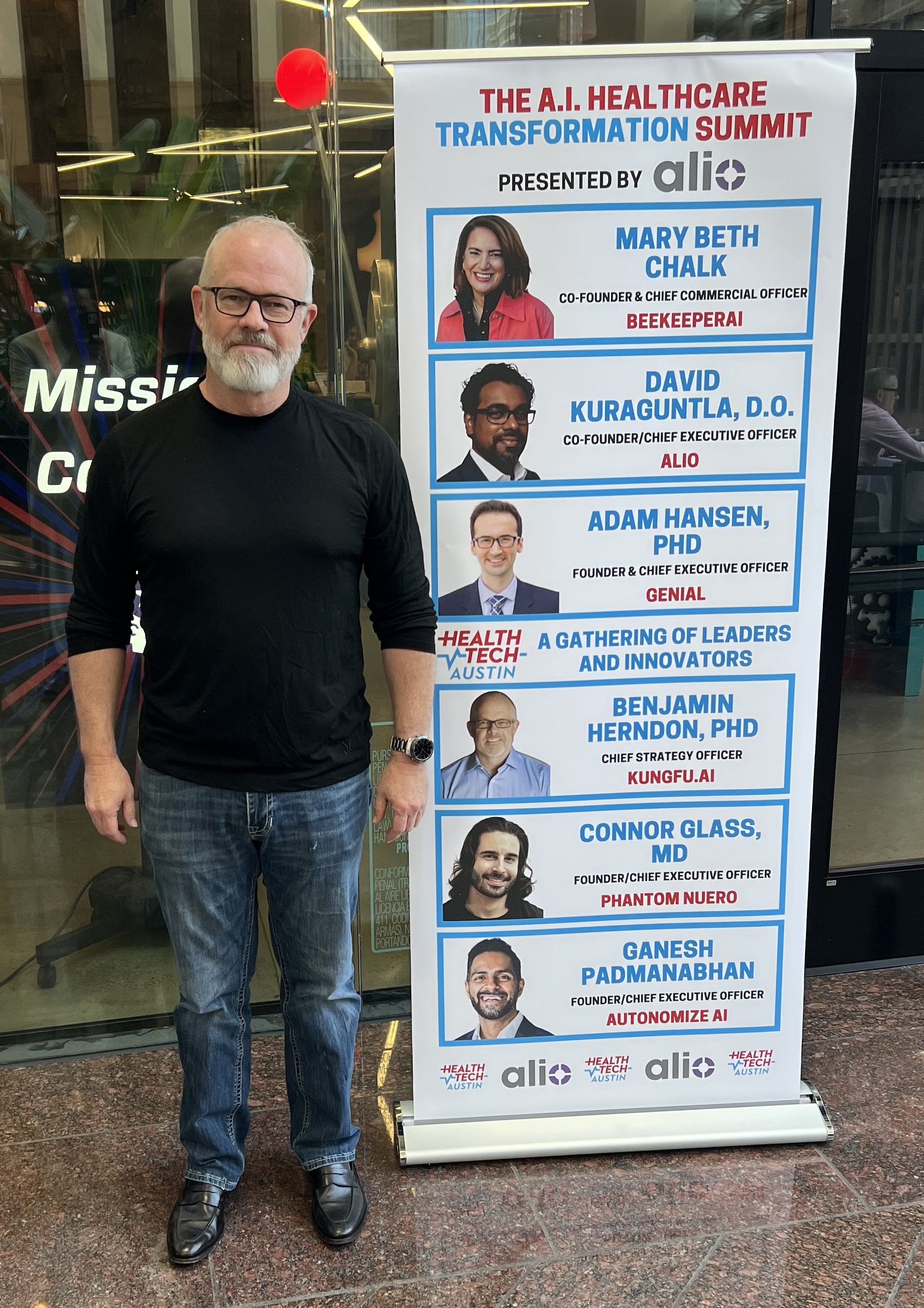
THOUGHT LEADERS AND INNOVATORS came TOGETHER TO SHARE THEIR KNOWLEDGE, EXPERIENCE, RESEARCH, AND INSIGHTS ABOUT a.I.
Presented by alio
summit recap
summit SPEAKERS
Elizabeth Jennings has worked at the intersection of international investment and commercialization within healthcare for the last fifteen years, spanning 28 countries and all classes of complexity, building a reputation for strategic risk management for both investors and companies.She is currently the Vice President of Marketing for an Australian Stock Exchange-traded AI company, Echo IQ, focused on leveraging AI in a proprietary manner to change the way structural heart diseases are detected.
Elizabeth has been a commercial leader at four AI healthtech startups and has consulted and advised dozens around the globe. She also serves on the Board of Directors for the fastest-growing angel impact network in the US, SWAN Impact; has led the European Network of Research Innovation Centres and Hubs' healthcare portfolio in the US; and served on multiple international healthcare councils, federal early-stage grant review panels, and accelerators.
Prior to joining Echo IQ, Elizabeth was the Managing Partner of Venture Atlas Labs, a commercialization firm known for bringing innovative technologies to commercial success in some of the most challenging markets around the world on behalf of family offices, private equity, VCs, and government funds. Her recent book, US Digital Healthcare Procurement, was commissioned by the Ministry of Foreign Affairs of Denmark and is a leading resource for navigating the US healthcare landscape for international startups.
Previous roles have included leading innovation programs for foreign governments at the Global Innovation Lab at the University of Texas at Austin, commercial expansion for multiple large diagnostics corporations in the US and France, and upstream investments in neglected tropical disease research.
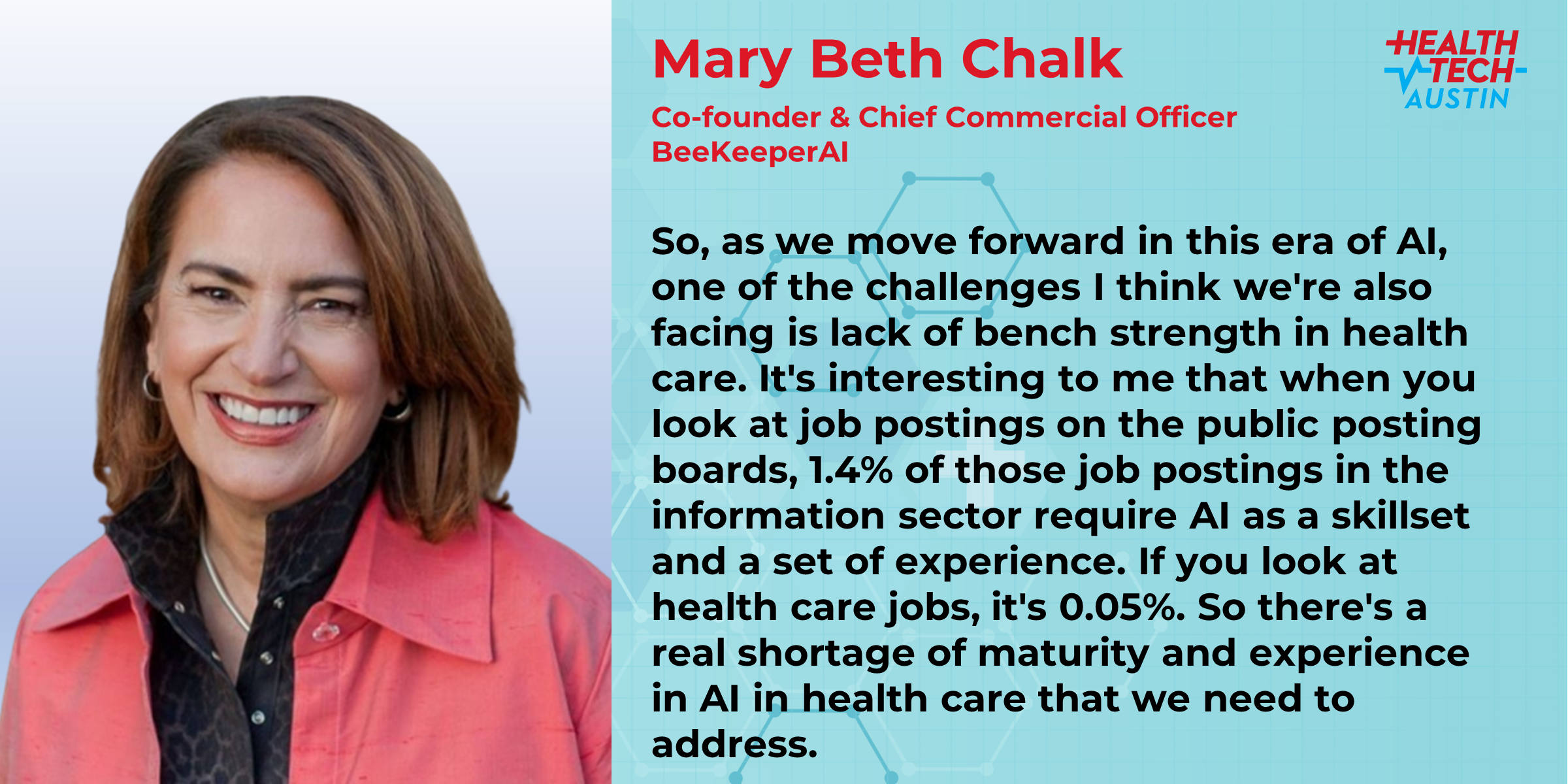
Mary Beth Chalk is the Co-founder and Chief Commercial Officer of BeeKeeperAI TM , creator of EscrowAI TM , a zero-trust, multi-party collaboration platform leveraging Azure confidential computing to enable end-to-end encryption for privacy protected information and the intellectual property of algorithm and analytic models. Mary Beth has over 25-years of creating and commercializing data-driven healthcare innovation.
Prior to BeeKeeperAI she led business development at the Center for Digital Health Innovation at UCSF where she secured over $50M in funding for innovation projects, including AI validation. Prior to UCSF, she was the Co-founder and Chief Engagement Officer for an AI platform spun out of Mass General Brigham delivering precision disease management coaching utilizing remote monitoring device data and social determinants of health.
During her tenure as the Chief Operating Officer of a mental health company she created and deployed the SIGNAL system (outcome prediction algorithms) utilized to inform and improve the effectiveness of psychotherapy.
David Kuraguntla, D.O. is the Co-Founder and CEO of Alio Medical. Dave received his master’s degree from Boston University and was a researcher at the National Institutes of Health. He then went to medical school on an Air Force scholarship.
He received his medical degree in osteopathic medicine (D.O.) and was preparing for a surgical residency when he experienced firsthand the need for better technological solutions for patients with chronic conditions. This experience lead Dave to start Alio, which has grown to become the best-in-class wearable system to remotely, non-invasively measure the function of the kidney, heart, and blood vessels.
The Alio SmartPatch synthesizes multiple, novel metrics to drive insights across cardiovascular and renal medicine, with special dedication to improving the lives of those living with chronic kidney disease (CKD).
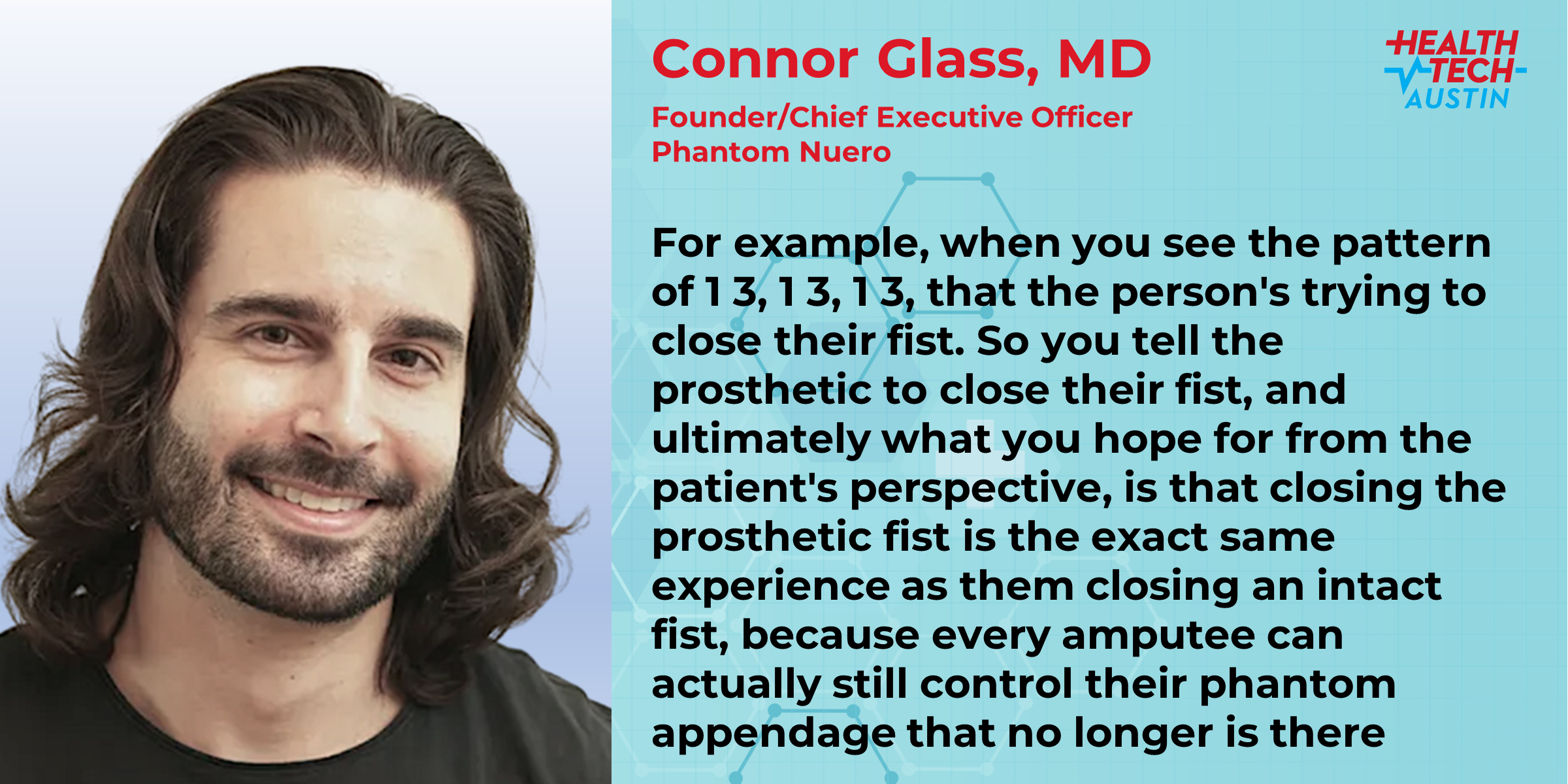
Dr. Connor Glass is the Founder & CEO of Phantom Neuro which seeks to enable lifelike control of prosthetic limbs and exoskeletons for individuals with limb difference and beyond. Dr. Glass received his medical degree from the University of Oklahoma College of Medicine followed by a multi-year research fellowship in Plastic Surgery at Johns Hopkins University School of Medicine where he studied surgical interventions for peripheral nerve injury and advanced prosthesis control.
He is the primary inventor of a minimally invasive implantable muscle-machine interface which his company now seeks to commercialize. His company has raised nearly $10 million in venture capital. Dr. Glass has multiple publications on nerve injury and neuromuscular reconstructive surgery and co-authored a chapter in the Handbook of Neuroengineering.
He works on domestic and international efforts to advance amputation care and prosthetic outcomes, and his work has been featured in outlets such as the Wall Street Journal, Axios, and STAT.
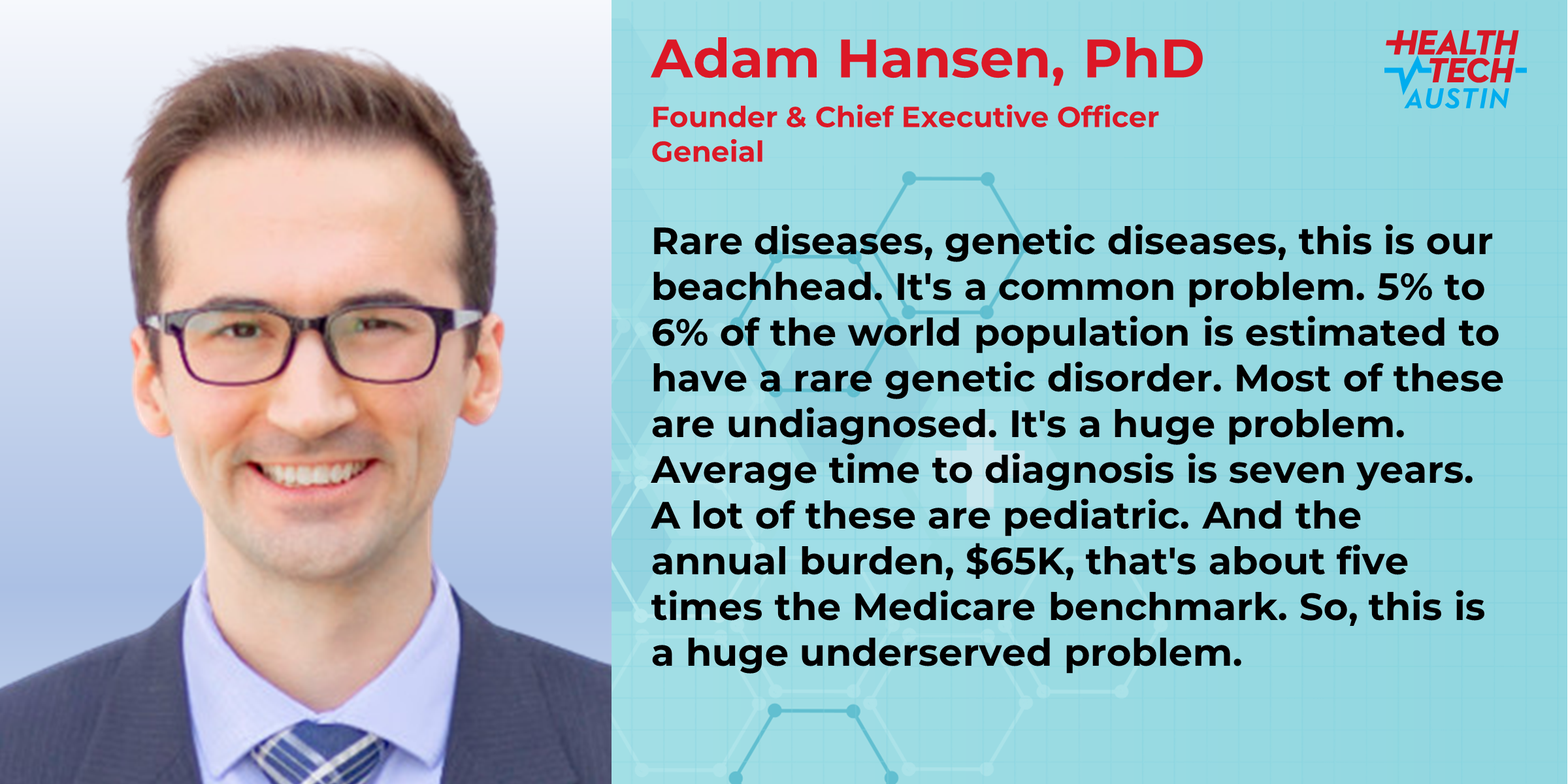
Dr. Adam Hansen is an accomplished scientist and entrepreneur who has dedicated his career to relieving human suffering through the advancement of precision medicine. He founded and leads Geneial, a private exchange for genetic and patient-reported outcomes data. Less than two years after completion of his doctoral training, Dr. Hansen and team were awarded a $2.3M fast-track Small Business Innovation Research (SBIR) grant from the National Human Genome Research Institute (NHGRI). He serves as Principal Investigator (PI), Founder, and CEO at Geneial and is a co-inventor of three international patent applications (pending).
During his doctoral training at Baylor College of Medicine under Dr. Richard Gibbs at the Human Genome Sequencing Center, he led the discovery of 154 candidate genetic disorders through a genocentric, query-optimization strategy for exome sequencing data of over 18,000 individuals. Upon completion of his doctoral studies, Dr. Hansen was selected as a Biodesign Fellow at the Texas Medical Center Innovation Institute, where he expanded his knowledge of digital health, value-based-care, and new venture formation.
Dr. Hansen’s research interests are focused on identifying novel genetic causes of human disease through next-generation sequencing, elucidating the natural history of genetic disorders through registry design and patient-reported outcomes data, data standardization, Mendelian and population genetics, pharmacogenomics, and high-performance computing. He is passionate about leveraging AI to accelerate the pace of discovery, aligning incentives for data exchange, and enhancing protections for patient privacy and data ownership.
He received a Bachelor of Science in Bioinformatics from Brigham Young University with minors in Computer Science, Chinese, and Global Business & Literacy. He also studied abroad at Nanjing University, where he studied advanced Chinese Language and Literature, and is fluent in Mandarin. In his free time he volunteers to teach a weekly English as a Second Language (ESL) course. He serves on the industry advisory board for the University of Utah Department of Biomedical Informatics, and has been invited to speak on health equity, innovation, and the importance of character in leadership.
Dr. Ben Herndon, Chief Strategy Officer at KUNGFU.AI has over 30 years of experience in organizational transformation and cognition. He has worked with organizations ranging from small startups to the U.S. Internal Revenue Service, where he was the first Chief Research and Analytics Officer leading the operationalization of AI/ML/DS at scale in tax collection.
Ben holds a Ph.D. in Organizational Cognition from the University of Texas at Austin McCombs School of Business and was a research professor at the Georgia Institute of Technology.
In his most recent role, he was Director of AI Strategy for Vista Equity Partners. He holds a B.S. in political science from Harvard University.
Ganesh Padmanabhan is the CEO & founder of Autonomize AI, a technology company applying Trusted Generative AI to healthcare and lifesciences. Autonomize’s AI products organize, contextualize and summarize unstructured data so healthcare knowledge workers can make data-driven decisions, to improve patient outcomes. Autonomize AI is a founding member of CancerX, US President Biden’s Cancer Moonshot initiative.
He is also the Founder & Chief Creator of Stories in AI, an edu-tainment venture. He previously co-founded and scaled Molecula Corp, a data management company, and led growth and commercial at CognitiveScale, Inc, an Enterprise AI company. Prior to that he spent a 15 year career spanning Dell Technologies and Intel Corp.
A frequent keynote speaker, he is published at Forbes, Business Insider, Fast Company and other publications and was honored by the Enterprise Management 360 as one of the top 10 tech experts revolutionizing AI. Ganesh holds a bachelor’s degree in Mechanical Engineering from University of Calicut, India, and an MBA from McCombs School at the University of Texas Austin.